Various types of organized lymphoid tissues are located
along the vessels of the lymphatic system. Some lymphoid tissue in the lung and
lamina propria of the intestinal wall consists of diffuse collections of
lymphocytes and macrophages. Other lymphoid tissue is organized into structures
called lymphoid follicles, which consist of aggregates of lymphoid and
nonlymphoid cells surrounded by a network of draining lymphatic capillaries.
Until it is activated by antigen, a lymphoid follicle—called a primary
follicle—comprises a network of follicular dendritic cells and small resting B
cells. After an antigenic challenge, a primary follicle becomes a larger
secondary follicle—a ring of concentrically packed B lymphocytes surrounding a
center (the germinal center) in which one finds a focus of proliferating B
lymphocytes and an area that contains nondividing B cells, and some helper T
cells interspersed with macrophages and follicular dendritic cells (Figure
2-17).
Most antigen-activated B cells divide and differentiate into
antibody-producing plasma cells in lymphoid follicles, but only a few B cells
in the antigen-activated population find their way into germinal centers. Those
that do undergo one or more rounds of cell division, during which the genes
that encode their antibodies mutate at an unusually high rate. Following the
period of division and mutation, there is a rigorous selection process in which
more than 90% of these B cells die by apoptosis. In general, those B cells
producing antibodies that bind antigen more strongly have a much better chance
of surviving than do their weaker companions. The small number of B cells that
survive the germinal center’s rigorous selection differentiate into plasma
cells or memory cells and emerge.
Lymph nodes and the spleen are the most highly organized of
the secondary lymphoid organs; they comprise not only lymphoid follicles, but
additional distinct regions of Tcell and B-cell activity, and they are
surrounded by a fibrous capsule. Less-organized lymphoid tissue, collectively
called mucosal-associated lymphoid tissue (MALT), is found in various body
sites. MALT includes Peyer’s patches (in the small intestine), the tonsils, and
the appendix, as well as numerous lymphoid follicles within the lamina propria
of the intestines and in the mucous membranes lining the upper airways,
bronchi, and genital tract.
LYMPH NODES
Lymph nodes are the sites where immune responses are mounted
to antigens in lymph. They are encapsulated beanshaped structures containing a
reticular network packed with lymphocytes, macrophages, and dendritic cells.
Clustered at junctions of the lymphatic vessels, lymph nodes are the first
organized lymphoid structure to encounter antigens that enter the tissue
spaces. As lymph percolates through a node, any particulate antigen that is
brought in with the lymph will be trapped by the cellular network of phagocytic
cells and dendritic cells (follicular and interdigitating). The overall
architecture of a lymph node supports an ideal microenvironment for lymphocytes
to effectively encounter and respond to trapped antigens.
Morphologically, a lymph node can be divided into three
roughly concentric regions: the cortex, the paracortex, and the medulla, each
of which supports a distinct microenvironment (Figure 2-18). The outermost
layer, the cortex, contains lymphocytes (mostly B cells), macro-phages, and
follicular dendritic cells arranged in primary follicles. After antigenic
challenge, the primary follicles enlarge into secondary follicles, each
containing a germinal center. In children with B-cell deficiencies, the cortex
lacks primary follicles and germinal centers. Beneath the cortex is the
paracortex, which is populated largely by T lymphocytes and also contains
interdigitating dendritic cells thought to have migrated from tissues to the
node. These interdigitating dendritic cells express high levels of class II MHC
molecules, which are necessary for presenting antigen to TH cells. Lymph nodes
taken from neonatally thymectomized mice have unusually few cells in the
paracortical region; the paracortex is therefore sometimes referred to as a
thymus-dependent area in contrast to the cortex, which is a thymus-independent
area. The innermost layer of a lymph node, the medulla, is more sparsely
populated with lymphoid-lineage cells; of those present, many are plasma cells
actively secreting antibody molecules. As antigen is carried into a regional
node by the lymph, it is trapped, processed, and presented together with class
II MHC molecules by interdigitating dendritic cells in the paracortex,
resulting in the activation of TH cells. The initial activation of B cells is
also thought to take place within the T-cell-rich paracortex. Once activated,
TH and B cells form small foci consisting largely of proliferating B cells at
the edges of the paracortex. Some B cells within the foci differentiate into
plasma cells secreting IgM and IgG. These foci reach maximum size within 4–6
days of antigen challenge. Within 4–7 days of antigen challenge, a few B cells
and TH cells migrate to the primary follicles of the cortex. It is not known
what causes this migration. Within a primary follicle, cellular interactions
between follicular dendritic cells, B cells, and TH cells take place, leading
to development of a secondary follicle with a central germinal center. Some of
the plasma cells generated in the germinal center move to the medullary areas
of the lymph node, and many migrate to bone marrow.
Afferent lymphatic vessels pierce the capsule of a lymph
node at numerous sites and empty lymph into the subcapsular sinus (see Figure
2-18b). Lymph coming from the tissues percolates slowly inward through the
cortex, paracortex, and medulla, allowing phagocytic cells and dendritic cells
to trap any bacteria or particulate material (e.g., antigen-antibody complexes)
carried by the lymph. After infection or the introduction of other antigens
into the body, the lymph leaving a node through its single efferent lymphatic
vessel is enriched with antibodies newly secreted by medullary plasma cells and
also has a fiftyfold higher concentration of lymphocytes than the afferent
lymph.
The increase in lymphocytes in lymph leaving a node is due
in part to lymphocyte proliferation within the node in response to antigen.
Most of the increase, however, represents blood-borne lymphocytes that migrate
into the node by passing between specialized endothelial cells that line the postcapillary
venules of the node. Estimates are that 25% of the lymphocytes leaving a lymph
node have migrated across this endothelial layer and entered the node from the
blood. Because antigenic stimulation within a node can increase this migration
tenfold, the concentration of lymphocytes in a node that is actively responding
can increase greatly, and the node swells visibly. Factors released in lymph
nodes during antigen stimulation are thought to facilitate this increased
migration.
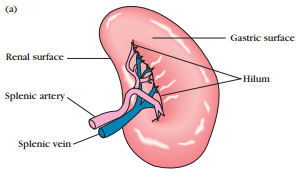
SPLEEN
The spleen plays a major role in mounting immune responses
to antigens in the blood stream. It is a large, ovoid secondary lymphoid organ
situated high in the left abdominal cavity. While lymph nodes are specialized
for trapping antigen from local tissues, the spleen specializes in filtering
blood and trapping blood-borne antigens; thus, it can respond to systemic
infections. Unlike the lymph nodes, the spleen is not supplied by lymphatic
vessels. Instead, bloodborne antigens and lymphocytes are carried into the
spleen through the splenic artery. Experiments with radioactively labeled
lymphocytes show that more recirculating lymphocytes pass daily through the
spleen than through all the lymph nodes combined.
The spleen is surrounded by a capsule that extends a number
of projections (trabeculae) into the interior to form a compartmentalized structure.
The compartments are of two types, the red pulp and white pulp, which are
separated by a diffuse marginal zone (Figure 2-19). The splenic red pulp
consists of a network of sinusoids populated by macrophages and numerous red
blood cells (erythrocytes) and few lymphocytes; it is the site where old and
defective red blood cells are destroyed and removed. Many of the macrophages
within the red pulp contain engulfed red blood cells or iron pigments from
degraded hemoglobin. The splenic white pulp surrounds the branches of the
splenic artery, forming a periarteriolar lymphoid sheath (PALS) populated
mainly by T lymphocytes. Primary lymphoid follicles are attached to the PALS.
These follicles are rich in B cells and some of them contain germinal centers.
The marginal zone, located peripheral to the PALS, is populated by lymphocytes
and macrophages.
Blood-borne antigens and lymphocytes enter the spleen
through the splenic artery, which empties into the marginal zone. In the
marginal zone, antigen is trapped by interdigitating dendritic cells, which
carry it to the PALS. Lymphocytes in the blood also enter sinuses in the
marginal zone and migrate to the PALS. The initial activation of B and T cells
takes place in the Tcell-rich PALS. Here interdigitating dendritic cells
capture antigen and present it combined with class II MHC molecules to TH
cells. Once activated, these TH cells can then activate B cells. The activated
B cells, together with some TH cells, then migrate to primary follicles in the
marginal zone. Upon antigenic challenge, these primary follicles develop into
characteristic secondary follicles containing germinal centers (like those in
the lymph nodes), where rapidly dividing B cells (centroblasts) and plasma
cells are surrounded by dense clusters of concentrically arranged lymphocytes.
The effects of splenectomy on the immune response depends on
the age at which the spleen is removed. In children, splenectomy often leads to
an increased incidence of bacterial sepsis caused primarily by Streptococcus
pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Splenectomy in
adults has less adverse effects, although it leads to some increase in
blood-borne bacterial infections (bacteremia).
MUCOSAL-ASSOCIATED LYMPHOID TISSUE
The mucous membranes lining the digestive, respiratory, and
urogenital systems have a combined surface area of about 400 m2
(nearly the size of a basketball court) and are the major sites of entry for
most pathogens. These vulnerable membrane surfaces are defended by a group of
organized lymphoid tissues mentioned earlier and known collectively as
mucosal-associated lymphoid tissue (MALT). Structurally, these tissues range
from loose, barely organized clusters of lymphoid cells in the lamina propria
of intestinal villi to well-organized structures such as the familiar tonsils
and appendix, as well as Peyer’s patches, which are found within the submucosal
layer of the intestinal lining. The functional importance of MALT in the body’s
defense is attested to by its large population of antibody-producing plasma
cells, whose number far exceeds that of plasma cells in the spleen, lymph
nodes, and bone marrow combined.
The tonsils are found in three locations: lingual at the
base of the tongue; palatine at the sides of the back of the mouth; and
pharyngeal (adenoids) in the roof of the nasopharynx (Figure 2-20). All three
tonsil groups are nodular structures consisting of a meshwork of reticular
cells and fibers interspersed with lymphocytes, macrophages, granulocytes, and
mast cells. The B cells are organized into follicles and germinal centers; the
latter are surrounded by regions showing T-cell activity. The tonsils defend
against antigens entering through the nasal and oral epithelial routes.
The best studied of the mucous membranes is the one that
lines the gastrointestinal tract. This tissue, like that of the respiratory and
urogenital tracts, has the capacity to endocytose antigen from the lumen.
Immune reactions are initiated against pathogens and antibody can be generated
and exported to the lumen to combat the invading organisms. As shown in Figures
2-21 and 2-22, lymphoid cells are found in various regions within this tissue.
The outer mucosal epithelial layer contains so-called intraepithelial
lymphocytes (IELs). Many of these lymphocytes are T cells that express unusual
receptors ( T-cell receptors, or TCRs),
which exhibit limited diversity for antigen. Although this population of T
cells is well situated to encounter antigens that enter through the intestinal
mucous epithelium, their actual function remains largely unknown The lamina
propria, which lies under the epithelial layer, contains large numbers of B
cells, plasma cells, activated TH cells, and macrophages in loose clusters.
Histologic sections have revealed more than 15,000 lymphoid follicles within
the intestinal lamina propria of a healthy child. The submucosal layer beneath
the lamina propria contains Peyer’s patches, nodules of 30–40 lymphoid
follicles. Like lymphoid follicles in other sites, those that compose Peyer’s
patches can develop into secondary follicles with germinal centers.
The epithelial cells of mucous membranes play an important
role in promoting the immune response by delivering small samples of foreign
antigen from the lumina of the respiratory, digestive, and urogenital tracts to
the underlying mucosal-associated lymphoid tissue. This antigen transport is
carried out by specialized M cells. The structure of the M cell is striking:
these are flattened epithelial cells lacking the microvilli that characterize
the rest of the mucous epithelium. In addition, M cells have a deep
invagination, or pocket, in the basolateral plasma membrane; this pocket is
filled with a cluster of B cells, T cells, and macrophages (Figure 2-22a).
Luminal antigens are endocytosed into vesicles that are transported from the
luminal membrane to the underlying pocket membrane. The vesicles then fuse with
the pocket membrane, delivering the potentially response-activating antigens to
the clusters of lymphocytes contained within the pocket.
M cells are located in so-called inductive sites—small
regions of a mucous membrane that lie over organized lymphoid follicles (Figure
2-22b). Antigens transported across the mucous membrane by M cells can activate
B cells within these lymphoid follicles. The activated B cells differentiate
into plasma cells, which leave the follicles and secrete the IgA class of
antibodies. These antibodies then are transported across the epithelial cells
and released as secretory IgA into the lumen, where they can interact with
antigens.
As described in Chapter 1, mucous membranes are an effective
barrier to the entrance of most pathogens, which thereby contributes to
nonspecific immunity. One reason for this is that the mucosal epithelial cells
are cemented to one another by tight junctions that make it difficult for
pathogens to penetrate. Interestingly, some enteric pathogens, including both
bacteria and viruses, have exploited the M cell as an entry route through the
mucous-membrane barrier. In some cases, the pathogen is internalized by the M
cell and transported into the pocket. In other cases, the pathogen binds to the
M cell and disrupts the cell, thus allowing entry of the pathogen. Among the
pathogens that use M cells in these ways are several invasive Salmonella
species, Vibrio cholerae, and the polio virus.
Source : Richard A. Goldsby, Thomas J. Kindt, And Barbara A. Osborne. 2000. KUBY IMMUNOLOGY 4th Edition. New York. W. H. FREEMAN AND COMPANY. Page 46 - 52.






Wow such a nice post which you uploaded here. Thanks for sharing so nice article. It really helps me out.
BalasHapusNode.js Development Company |
Hire Node.js Developer